
Osteochondrosis is one of the most common pathologies of the spine. It is believed to mainly develop in the neck or lower back. After all, it is in these places that the spine is very mobile and subjected to great stress. But the sedentary lifestyle of most people and prolonged sitting at a table led to the fact that osteochondrosis of the thoracic spine began to occur more frequently. Although in many cases this pathology is not diagnosed immediately. After all, the peculiarity of thoracic osteochondrosis is that its symptoms are non-specific and reminiscent of many other pathologies.
general characteristics
This degenerative-dystrophic disease affects the intervertebral discs of the thoracic spine. This is due to the violation of metabolic processes, which leads to thinning and drying of the cartilage tissue. As a result, under the influence of physical exertion, the discs begin to collapse and lose their damping functions. The vertebrae, ligaments and joints in the spine are gradually affected. Nerve fibers and blood vessels can be damaged.
This process develops slowly, so the pathology is difficult to diagnose. Moreover, not everyone goes to the doctor immediately, because they do not know what the danger of thoracic osteochondrosis is. But without treatment, the disease can lead to serious complications. Because this part of the spine is responsible for the blood supply and innervation of internal organs, various pathologies can develop in the advanced form of osteochondrosis of the thoracic spine. Intestinal peristalsis, heart, liver and digestive tract disorders are disturbed. Pancreatitis, cholecystitis, biliary dyskinesia may occur. But most often complications occur in the spine. In addition to intervertebral disc herniation and intercostal neuralgia, spinal cord compression, spondylosis, sciatica, and postural disorders may develop.
Osteochondrosis of the thoracic spine is equally common in men and women. Its appearance does not even depend on age, although it was previously believed that degenerative-dystrophic diseases are characteristic only of the elderly. But modern youth are increasingly suffering from osteochondrosis due to improper diet and sedentary lifestyle.
The most common osteochondrosis is thought to be cervical. Often the pathology also occurs in the lumbar region. This is due to the special structure of the skeleton. In the thoracic part, the spine is less mobile, because it is connected to the ribs and sternum.
The intervertebral discs are thinner here, and the vertebrae are closer together. But this part is less susceptible to injuries and other external influences, because part of the load is taken by the ribs and chest.
Osteochondrosis usually occurs at the level of 7-11 vertebrae. In this case, the intervertebral discs are primarily affected. 1-2 segments of the spine are most often affected. But sometimes polysegmental osteochondrosis develops, in which several discs are destroyed at the same time. Rarely, the pathology in this part occurs on its own, usually in combination with a lesion of the cervical or lumbar spine. In this case, the symptoms are more pronounced, so it becomes easier to diagnose the disease.
The peculiarity of thoracic osteochondrosis is that it rarely manifests as back pain after exertion, as is the case when it is localized in the cervical or lumbar spine. In the initial phase, the pathology is confused with heart or lung diseases. After all, the pain is often localized in the chest, there is difficulty breathing, nausea, chills. But the manifestations of thoracic osteochondrosis are not very bright, so patients do not always go to the doctor in the initial stage. Due to that, the pathology progresses.
Disease development
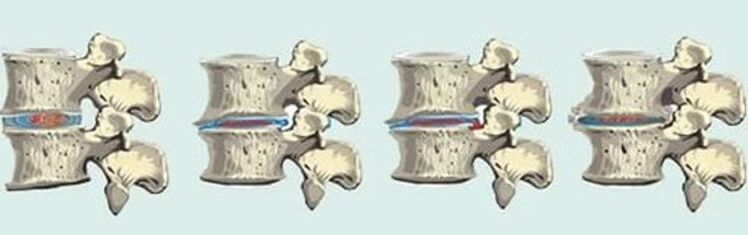
The danger of thoracic osteochondrosis is that it "disguises" itself in other diseases. The pathology develops slowly, rarely any of the patients visit the doctor in the initial stage. Osteochondrosis begins with thinning of the intervertebral disc. Its core flattens, the shell cracks and dries, and the vertebrae approach. At this stage there is usually no major discomfort, only a slight muscle tension. If the disease can be detected, then it can be completely cured by restoring the condition of the discs.
But usually the progression of osteochondrosis continues. In the surrounding soft tissues, an inflammatory process can begin, the joint capsules suffer. The mobility of the spine is reduced, the vertebrae can be moved. If the increased physical activity continues, due to the friction of the vertebrae against each other, microcracks appear on them. At this point there is a feeling of tightness in the chest, pain with any movement in the upper body.
In the third phase of osteochondrosis, the intervertebral discs become very thin, bulges and hernias appear. The mobility of the spine is almost completely limited. Osteophytes begin to form on the vertebrae. This phase is characterized by a pronounced radicular syndrome, because the nerve fibers are damaged. In this case, the work of internal organs is seriously disturbed. In most cases, at that time the patient goes to the doctor and starts treatment. If this is not done, complications can lead to disability, and when the spinal cord is compressed, to complete immobility.
The last stage of osteochondrosis is characterized by complete destruction of the discs and loss of their functions. The bone tissue of the vertebrae begins to collapse, so the mobility of the spine is completely disrupted. All vegetative and radicular symptoms of thoracic osteochondrosis are clearly expressed.

The development of thoracic osteochondrosis is wavy. This is usually a chronic process that takes place slowly, with little discomfort. Increased fatigue, weakness may occur. And when exposed to external factors, it gets worse with sharp pains. In this case, patients are often hospitalized, as the attack may be accompanied by a feeling of shortness of breath, difficulty breathing, chest or abdominal pain.
Causes
The main cause of thoracic osteochondrosis, as in other forms, is a violation of mineral metabolism. As a result of degenerative-dystrophic processes, a protrusion or herniated disc appears, they become thinner and cease to perform their functions, the vertebrae gradually collapse, osteophytes grow. This is most often caused by an unbalanced diet, which leads to a lack of essential nutrients, or changes in the composition of cartilage tissue due to age. Disc degeneration can also lead to poor circulation in the spine, bad habits, or a hereditary predisposition.
But mineral deficiency does not always lead to osteochondrosis. This requires provoking factors that affect the spine itself.
Therefore, the following reasons for this pathology also differ:
- frequent static loads on the spine;
- prolonged sitting in an uncomfortable position at a table;
- weightlifting;
- obesity;
- injury to the spine or surrounding tissue;
- engaging in strength sports;
- rachiocampsis;
- muscle corset weakness;
- congenital skeletal malformations;
- severe hypothermia;
- nervous strain.

It turns out that people who spend a long time in an awkward position at a table or driving a car, as well as those who perform hard physical work, are most susceptible to the development of pathology. Indeed, both increased loads and their complete absence are equally detrimental to intervertebral discs.
In addition, osteochondrosis often develops in young people who have osteochondropathy. This pathology usually develops in the lower chest in adolescents. It is characterized by necrosis of the spongy tissue of the vertebrae, spinal deformity and the appearance of neurological symptoms. With the progression of the pathology, osteochondrosis becomes complicated.
Manifestations of pathology
The main symptoms of thoracic spine osteochondrosis are pain, radicular syndrome, and dysfunction of internal organs. The pain in this pathology can be sharp, paroxysmal or painful, constant, increasing with movement. Sometimes patients are admitted to the hospital with suspicion of acute pancreatitis, cholecystitis or urolithiasis. After all, the pain is not always localized in the area of the affected vertebrae. Therefore, osteochondrosis of the chest is often mistaken for pathologies of other organs.
In addition, degenerative processes in the spine in this disease are almost always accompanied by vascular disorders or intercostal neuralgia. This is due to the special structure of the spine in this part - the small distance between the vertebrae and the large number of nerves and blood vessels.

Thoracic osteochondrosis may be suspected of limited mobility of the upper body, increased curvature. Intercostal neuralgia often occurs. Acute pain can last for hours or longer. It can be stimulated by lifting weights, long-term retention of static position, hypothermia.
If the veins are affected, there is a violation of the blood supply and nutrition of the skin. This results in increased nail fragility, dryness and flaking of the skin. Cold skin and cold limbs are often observed.
Characteristics of pain
Pain in osteochondrosis of the thoracic region can vary in intensity and location. The pain usually occurs in the chest or between the shoulder blades. They are intensified by raising the arm, turning or bending the body, coughing or sneezing. The pain can be sharp, pressing, aching.
Usually such feelings are divided into two groups: dorsago and dorsalgia. Dorsago is an attack of acute pain between the shoulder blades. It is also called "chest lumbago". The pain is so strong that it prevents the person from moving. A dorsal attack usually occurs after a long stay in a stationary position during the first movement. It is followed by muscle spasm, so respiratory function is disturbed. The sensation extends to the shoulder blade, between the ribs to the chest. Chest pain in osteochondrosis is reminiscent of an attack of angina pectoris, but unlike it, nitroglycerin does not remove it. In addition, the pain increases when the vertebrae are pressed.
Dorsalgia is a chronic, mild pain. It usually begins gradually, with mild discomfort in the thoracic spine. In this case, the pain may increase when bending, turning, raising the arm, and even when walking. This severely limits the patient's mobility. In addition, an increase in pain may be noticed on deep breathing, after a long stay in a sitting position, or at night. Dorsalgia can last from 2 weeks to a month. Chest tightness and shortness of breath may resemble pneumonia, but the patient does not have a cough or fever.

Radicular syndrome
When the vertebrae or spasmodic muscles of the nerve roots are compressed, the signs of osteochondrosis of the thoracic region become more pronounced. After all, the spinal nerves located at this site of the spine are responsible for the innervation of the skin, the motor functions of the limbs, and the functioning of the internal organs.
In addition to shooting pains in the back, chest or abdomen, nerve compression is accompanied by the following symptoms:
- paresis or partial paralysis of the limbs;
- violation of skin sensitivity;
- numbness, tingling, stinging, feeling of running "goose";
- violation of tendon reflexes;
- reflex muscle spasm;
- trophic changes in the skin - hair loss, discoloration, dryness and dandruff.
The intensity of these symptoms increases with physical exertion, deep breathing, prolonged sitting, after hypothermia or stress.

Vegetative disorders
The thoracic spine contains a lot of nerves and blood vessels that ensure the normal functioning of internal organs. Therefore, various autonomic disorders are necessarily observed in osteochondrosis. They depend on the localization of the affected vertebrae as well as on the stage of the pathology.
In spinal lesions in the upper thoracic part, there is discomfort in the esophagus, a feeling of coma in the throat. Difficulty swallowing, voice changes may occur. The middle thoracic vertebrae are responsible for the liver, gallbladder, stomach, and pancreas. Therefore, when destroyed, the symptoms often appear similar to pancreatitis, cholecystitis or gastritis. If degenerative changes have affected the lower thoracic vertebrae, problems with the intestines and genitals can occur.
Patients often consult a doctor with abdominal pain. They usually get worse in the evening or after physical work. Moreover, pain is not related to the characteristics of the patient’s diet. This gastrological syndrome is characteristic of thoracic osteochondrosis. But despite abdominal pain, bowel disorders, nausea and bloating, problems with the functioning of the digestive tract were not found. These feelings are caused by damage to the nerves and blood vessels in the spine.
Diagnosis
Due to the fact that the signs of osteochondrosis of the chest are nonspecific, the pathology can be detected only by a comprehensive examination. At the same time, it is very important to distinguish it from other diseases. X-ray or tomography of the spine helps to rule out spondylopathy, rheumatoid arthritis, ankylosing spondylitis.
But other testing methods are needed. This is a urine analysis, general and biochemical blood test, fluorography, ECG, MRI or ultrasound of internal organs. Such an examination enables the exclusion of pathologies such as pancreatitis, gastritis, gastric ulcer, heart attack, pneumonia and urolithiasis.

Treatment
Treatment of thoracic spine osteochondrosis should be comprehensive. Since the cause of the pathology is degenerative processes, it is impossible to completely cure it. Only in the initial stage, while the structure of the spine is not yet disturbed, and the discs are only slightly reduced, this process can be stopped and the functions of the spine restored.
But usually the treatment of osteochondrosis of the chest is aimed at slowing down the destruction of tissue, relieving pain and neurological symptoms, and restoring mobility. The choice of therapeutic methods depends on the stage of pathology, the localization of degenerative processes, the symptoms that are manifested. It is necessary to start treatment as soon as possible, then there are more possibilities to avoid complications.
It is especially important to see a doctor when your back hurts a lot and the shooting pain spreads to your chest or shoulder blade. Such deterioration can be removed by special methods. These are usually drugs used in the form of tablets or injections, various ointments or compresses, physiotherapy procedures. It is also necessary to immobilize the spine: the patient is shown resting in bed and restriction of movement for several days.
After the attack is removed, the treatment is not stopped. But now its main goal is to stop degenerative processes and restore tissue trophism. Among the drugs used for this are hydroprotectors, vitamins and means to improve metabolism. In addition, courses in massage and physiotherapy procedures, as well as physiotherapy exercises, must be prescribed. Moreover, performing special exercises should be constant. To prevent complications, it is necessary to monitor the diet so that it supplies the body with all the necessary vitamins and minerals. Lifestyle is also very important: choosing the right mattress and pillow for sleeping, chairs for work, alternating between rest and physical activity.
Chest osteochondrosis is a rather serious pathology which, if left untreated, can lead to dangerous complications. But difficulties in diagnosis lead to the fact that the disease often progresses. That’s why it’s so important to lead a proper lifestyle and avoid the factors that cause disk destruction. This will prevent the development of osteochondrosis and keep the spine healthy.

























